Governor Signs Long Term Care Legislation
On September 26, Governor Maura Healey ceremonially signed milestone legislation reforming the long-term care sector in Massachusetts. On September 6, she officially signed into law H 5033, An Act to improve quality and oversight of long-term care, as Chapter 197 of the Acts of 2024.
DignityMA released statement: Milestone long-term care reform legislation signed into law praised by Dignity Alliance Massachusetts
Among its many provisions, the law strengthens the licensure process for long-term care facilities under the jurisdiction of the Department of Public Health (DPH). Each of the 345 nursing homes in the Commonwealth will be inspected at least once every nine to 15 months and the schedule of financial penalties has been increased for the first time in decades.
Management and ownership transparency and accountability have been increased. Owners or management companies with at least 5 percent controlling interest in a facility are required to disclose pertinent information to DPH, including criminal and civil litigation histories, statements of financial capacity, bankruptcy filings, loan defaults, the appointment of a receiver, and the recording of a lien.
“Chapter 197 is the most significant law affecting long-term care enacted In over four decades,” Lanzikos noted. “This is the first phase of three to ensure that nursing home residents and staff receive high-quality, safe, and personalized care. This step must be followed up with the promulgation of comprehensive and robust regulations by DPH and other state agencies as soon as possible. Most importantly, the law and regulations must be rigorously enforced in a timely manner. Massachusetts’ older and disabled residents deserve nothing less.”
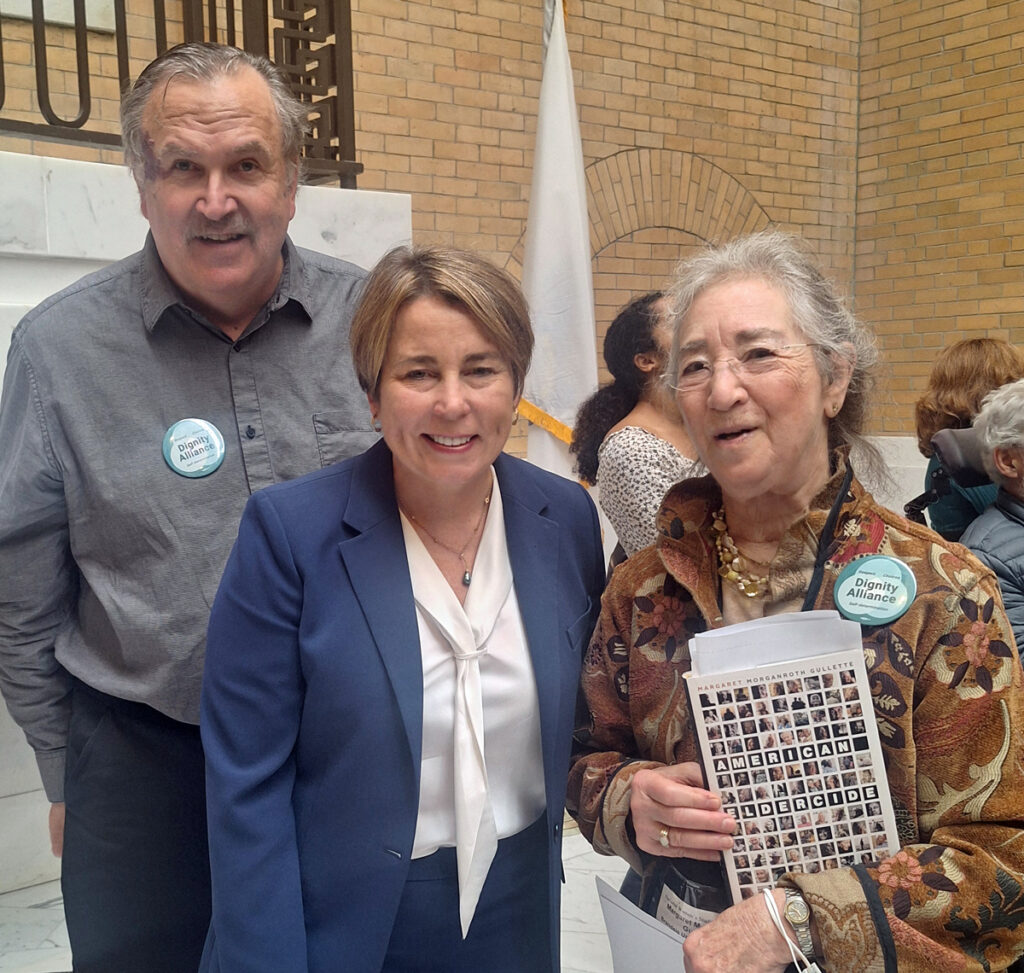
Photo: Paul, Governor Healey and Margaret at signing.
House and Senate approve Long Term Care Legislation
On August 29, 2024, the Massachusetts House and Senate each unanimously approved the omnibus long-term care legislation, H.5033.
The many provisions of this bill have been the focus of DignityMA’s advocacy throughout this legislative session. We thank the members of the conference committee, Speaker Marino, President Spilka, Ways and Means Chairs Rodrigues and Michlewitz, and especially the Co-Chairs of the Joint Committee on Elder Affairs, Senator Patricia Jehlen and Representative Thomas Stanley for their leadership.
We are especially grateful to all the DignityMA participants and supporters who added their voices to help get this milestone legislation passed.
Scroll Down for DignityMA’s media release and initial analysis of the bill as well as remarks made by Senator Jehlen during today’s Senate session.
August 30: Boston Globe Editorial “A step toward ending nursing home horror stories” asks Governor Healey to sign the bill.
Statement of Dignity Alliance Massachusetts on the Passage of the Long-Term Care Bill
Dignity Alliance Massachusetts commends the Long-Term Care Bill (H.5033) Conference Committee members, Speaker Mariano, and President Spilka for their efforts to continue resolving differences in the House and Senate versions of the bill even after the end of formal sessions. We especially thank the architects of the bill, the Co-Chairs of the Joint Committee on Elder Affairs, Senator Patricia Jehlen and Representative Thomas Stanley.
Since each previous version – S2889 and H4193 – received unanimous support from their respective chambers, we applaud the Legislature for sticking to their work and producing a bill that significantly advances the urgent need for long-term care reform. In any legislation of this magnitude, there will likely be the need to make further improvements in the future, nonetheless this bill represents a strong start toward the needed transformational reform of the long-term care industry.
The bill released by the Conference Committee, which we expect the Legislature to speedily enact and be signed by Governor Healey, represents a commitment to older adults and people with disabilities for improvements in care and safety. However, that set of bold promises will be hollow unless the Department of Public Health and Division of Insurance issue strong, effective regulations to implement the various provisions, and vigorously enforce them in the coming months.
“Residents of nursing homes and assisted living facilities will, we expect, soon see the improvements in their care, as long as state officials take the necessary steps to enforce the provisions of this bill. We are pleased with the changes to licensing and ownership requirements that make long-term care a system that places the health and well-being of older adults and persons with disabilities above the profits of private equity and other ownership interests,” explained, Paul J. Lanzikos, Dignity Alliance Coordinator and c0-founder. He is also a former Secretary of the Executive Office of Elder Affairs and a member of the Massachusetts Public Health Council.
Arlene German, a co-founder of both Dignity Alliance and Massachusetts Advocates for Nursing Home Reform (MANHR) said, “This bill includes numerous improvements in long-term care, some of which, MANHR has worked to implement for twenty years. Sadly, it took a pandemic and the deaths of many nursing home residents, to bring attention to the suffering of nursing home residents and provide an impetus for reforms.”
“Reform of long-term care in Massachusetts, has been, and continues to be, a top priority for Dignity Alliance since our founding at the height of the COVID pandemic, we will monitor the implementation of this important measure as we plan our legislative agenda for the next term,” noted former Senator Richard T. Moore, a co-founder and Legislative Chair of Dignity Alliance. Moore also serves on the Leadership Council of the National Consumer Voice for Quality Long-Term Care.
DignityMA Initial Assessment
Dignity Alliance Massachusetts’ Overall assessment of Long-Term Care Bill (H.5033):
While the legislation is not transformative, it is positive movement toward enhanced transparency and accountability regarding long-term services, support, and care especially in nursing homes and assisted living residences.
Provisions we applaud:
- Study of eligibility of guardians as MassHealth providers
- Provisions regarding the use of pooled trusts for persons aged 65 years and older
- Limitations on estate recovery following death of Medicaid beneficiaries
- More robust oversight and involvement by the Attorney General
- Strengthened regulations regarding insurance coverage
- The schedule of monetary penalties has been increased (We would like to see higher amounts.)
Positive provisions that require further attention:
- Qualifications of specialty care programs covered by MassHealth must be defined through regulations promulgated by DPH. Regulations must be clear and definitive; regulations must be rigorously enforced.
- Capital advisory committee lacks input from advocates
- Ownership interest defined as 5% or more; there should be no minimum percentage or alternatively set at 1%
Concerns that need clarification:
- Limits on public availability about provider finances; minimally should be accessible for the purposes of research and analysis
- Pleased that private equity interests must be identified; not clear that requirement extends to real estate investment trusts which are prevalent in the nursing home sector
Related issues to be addressed:
- Wheelchair repair requirements
- Mandated use of air conditioning in nursing homes, congregate residences, and housing complexes for older adults and persons with disabilities
- Increase in personal needs allowance for nursing home residents to $160 monthly
- Enforcement of current minimum staffing regulations for nursing homes
- Appointment of permanent Secretary of Elder Affairs
- Re-establishment of the Secretary of Elder Affairs as a member of the Governor’s Cabinet
Closing thoughts:
Good legislation provides a strong foundation. However, robust and comprehensive regulations by operating agencies are essential accompanied by rigorous and timely enforcement. We will focus our attention on the development and enforcement of regulations.
Senator Patricia Jehlen’s Remarks on the Senate Floor
Statement of Senator Patricia Jehlen, Co-Chair, Joint Committee on Elder Affairs, regarding the passage of H 5033, the long term care reform bill.
This statement was made during the Senate session held on August 29, 2024.
Speaking over the phone, Sen. Jehlen said, Thank you, Mr. President. I wish I were there. It wouldn’t be so complicated. I’m so happy and grateful to be here virtually to take up this important and comprehensive bill. It incorporates several bills we worked on for many years. It will save lives and improve lives of residents and workers in long-term care facilities, provide more options for assisted living, and improve financing options for older people living with disabilities.
It’s such a complicated bill because it now includes several other bills. Most people don’t know about all the provisions so I’ll explain their importance, unfortunately at length. We don’t all agree on everything, but we have been able to reach an agreement that will help so many people. Thanks are also due to the many people who have called, written and testified about the conditions they’ve seen in too many nursing homes.
And finally, this would not have happened without the press covering stories of neglect and abuse. Many people were shocked by the groundbreaking Globe report starting in 2010 about the overuse of antipsychotic drugs for care and the expansion of for-profit chains. Most recently, there’s been a lot of regional coverage about homes in South Hadley and Northampton. And the Provincetown Independent has done deep reporting on poor care as well as finances of the area’s for-profit nursing home, the only one on the Cape within 30 miles.
There has been less coverage of the people in the homes that provide essential and excellent care. But anyone who has ever had a relative in a nursing home knows how vital good care is, and how crucial and often underappreciated and under-compensated individual caregivers are and I’ll always remember the CNA who helped make my father’s life more meaningful in his last year.
We’ve all been focused on the disaster of Steward hospitals. The trend toward for-profit companies gaining a larger and larger share of nursing homes, home care agencies and hospices is equally troubling and needs attention. They too often extract the value from these important organizations by cutting staff, not paying bills, selling the buildings to related REITs, and paying exorbitant fees and rents and then closing or being closed. In just 13 years, Massachusetts lost 23 percent of its nursing home beds, even while the population of older adults is growing fast.
The task force made recommendations to ensure the survival of essential quality homes with regional availability, while ensuring that those that closed in the future were those with low census and low quality. We issued the report, unfortunately in 2020 just before the pandemic, and then all of us focused on the immediate crisis during which up to one quarter of nursing facility residents died. The pandemic revealed starkly that nursing homes were unprepared to stop the spread of disease. Even nursing homes with high ratings lost many residents and workers.
The legislature has supported additional funding with some accountability on spending, and the Healey and Baker administrations have worked to keep essential nursing homes afloat while trying to ensure that those that enclosed were low quality and less regionally important.
Since the task force, 100 percent of the 31 closures — 31 closures in the last three and a half years — 100 percent of those closures have had one or two stars, the lowest ratings. But there’s a lot more that’s needed.
This bill will increase capital funding for nursing homes, and will require updating the base rate every two years. It will also expand the tools that DPH has by allowing more oversight and particularly the inclusion of suitability standards. Those standards will allow DPH to limit, restrict, suspend, or revoke a license, or deny a license or a license transfer. They can also appoint temporary facility managers for troubled facilities. It increases the civil penalties the attorney general can seek by 10 times. Instead of $25,000 for a death, it will go to $250,000. Also the fines that DPH can levy for noncompliance with regulations. Right now, the maximum fine is $50 a day, the same as the minimum fine for a speeding ticket. I want to recognize that gentleman from New Bedford who has pushed to increase fines and to require bed holds for many years. Finally, it also requires regular inspections and outbreak response plans, and sets standards for special care units. So, adequate and targeted payment, plus more accountability, is a major goal and what has been most focused on by the press.
But this bill also incorporates an assisted living bill, which will make permanent the temporary allowance for assisted living residences to offer basic health services. Assisted living residences are certified by Elder Affairs, not the Public Health Department, and they’re generally considered non-medical facilities. They all have nurses on staff, but they can’t do simple things like administering eye drops or insulin injections. So when someone needed those things, things most people can do for themselves or their family members, they had to hire another nurse or get family members to come in and help them, or they had to move to a nursing home at more expense, as well as the disruption of moving. During the pandemic, there has been a temporary allowance for assisted living nurses to provide those services. It expires next March. There have been no cases of bad results in those assisted livings that offer those services. This bill continues that option for assisted living residences to offer those services.
It also requires more disclosure of ownership, and provides for fines in case of failure to follow regulations.
Another bill we’ve worked on for years, incorporated in this one, requires regulations to create small house nursing homes which serve 14 or fewer residents in more home-like environments and more safety from disease and more dignity.
Yet another bill incorporated here is the LGBTQ bill of rights for nursing home residents, banning discrimination and requiring training of staff. And this came out of the work of the LGBTQ aging commission.
Another important bill incorporated here addresses special needs pooled trusts. People with disabilities under 65 can transfer their resources to a trust to reduce their assets so they can qualify for MassHealth. That money can be used for needs like home care, home adaptations, personal items, assisted living expenses. For 30 years, until this spring, MassHealth allowed seniors with disabilities to establish and use pooled trusts, and we need to restore that option. It’s important to notice that any unexpended money from these trusts is sent back to MassHealth when the person dies.
There’s a new requirement in the bill that insurers must approve or deny prior authorization for transfer of patients from hospitals to nursing homes within one business day. This will prevent the common experience of patients being stuck in hospitals waiting for insurance approval.
Finally, the bill limits estate recovery from Medicaid and common health recipients to the limits the federal government requires. This will prevent family members from losing their homes where they had cared for their disabled relatives, and prevent generational impoverishment.
The bill also creates task forces and studies to inform our next steps, that include task forces to examine issues like hospital throughput, long term care eligibility, rest homes, CCRCs, and further LR reforms.
We need to strengthen all the pieces of the entire continuum, from home care to adult day health to rest homes to assisted living to nursing homes, and we need to continue to address the workforce crisis. This is incredibly important, comprehensive and long-needed legislation.
But there’s much that remains. I hope the House passes, and we take up, the home care licensure bill. We need to make permanent the provision for holding beds for nursing home residents who leave for medical care, instead of making it depend on annual budgets. We need to increase the personal needs allowance, which has not been raised for over 30 years. We need to make sure DPH has the resources and the will to use the tools we are giving them to ensure quality care.
And finally, it’s important to restore the Elder Affairs secretary to the Cabinet. The Elder Affairs secretary is now the only secretary not in the Cabinet, and that role needs to have the recognition and the responsibility to bring the intersecting needs of older adults into all discussions.
Today is a wonderful and long-needed step forward, and I want to thank everyone involved and hope and expect it will be enacted today.
